Gig Harbor (253) 858-8100
Same Day Emergency Appointment Available
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.

There are a variety of skin conditions that affect the feet and can be quite threatening to the vitality of your feet. Plantar warts are one such condition. These warts can develop on the bottom of the feet when an individual is exposed to a form of human papillomavirus (HPV). This generally occurs from person-to-person contact or in warm, moist environments where HPV thrives. Plantar warts can be dangerous, potentially creating holes in the soles of the feet. Some individuals with plantar warts complain that the condition is quite itchy, and some report scratching at their plantar warts. Itchy plantar warts are not unusual. This is because the plantar wart is itself made up of dry skin that is flaking, which can be itchy. There are several things that you might be able to do at home to stop your plantar warts from itching. For example, you might be able to take an oatmeal bath to soothe the affected skin area. Additionally, you can try applying moisturizer to your plantar warts to get them to stop itching. The application of moisturizer can help replenish your feet with much-needed moisture, which can help the itching subside. Please see a podiatrist to learn more about how to treat your itchy plantar warts.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. James D. McAlexander from Gig Harbor Foot and Ankle Clinic. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
Treatment
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Gig Harbor, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
As you grow older, you will start to notice more problems with your feet due to wear and tear. This may also happen because the skin will start to become thin and lose elasticity. Some signs of aging feet are regular aches and pains, bunion development, and clawed toes.
Fortunately, there are ways you can improve comfort, relieve pain, and maintain mobility in your feet. One of the best ways to deal with aging feet is to exercise. If you keep active, your muscles will become toned which will then strengthen the arches in the foot and stimulate blood circulation.
It is important that you practice proper foot care to protect your aging feet. You should wash your feet in warm water on an everyday basis. Afterward, the feet need to be dried well and it is important to dry between the toes. Your toenails should be trimmed and kept under control; nails that are poorly cut may become ingrown. At the end of each day, performing an inspection of your feet will allow you to detect any ailments in their early stages.
As you grow older, it becomes more important that you wear comfortable shoes. Your shoes should be secure, and they should provide decent arch support. If you are looking to buy a new pair of shoes, it is best to look for a pair that are made from a breathable material. It is also helpful to have shoes that have a bit of extra room at the top of the shoe, especially if you suffer from swollen feet.
The most common foot problems that elderly people will encounter are bunions, calluses, corns, hammertoes, heel pain, and foot problems related to diabetes. Some other issues include arch pain, tarsal tunnel syndrome, Achilles tendonitis, and Morton’s neuroma
An annual foot examination is a great way for you to ensure that you do not have any serious health problems with your feet. You should talk to a podiatrist about the available treatment options for whichever foot issue you are dealing with.

As an individual ages, it becomes even more essential that they are able to maintain proper foot health. This is because if a senior citizen has significantly unhealthy feet, their freedom and independence will be substantially reduced. However, as an individual ages, they also become more susceptible to experiencing foot afflictions. Therefore, senior citizens who want to take extra care of their health should be proactive in maintaining good foot care. One way to do this is to have a set time daily or once each week to examine the feet. The senior can do this by themselves or by asking for the help of a friend. Simply examine the foot for any noticeable problems including redness, swelling, deformations, or complications in the toenails. Scheduling a kind of regular inspection can be helpful for seniors because it enables them to check for any potential problems before they become exacerbated with time. Additionally, to be proactive, seniors can be sure that the shoes that they are wearing are not restrictive or too tight. Wearing properly fitted footwear is essential when an individual ages because ill-fitting shoes can reduce blood circulation and facilitate other troublesome foot afflictions. If you are a senior, be especially diligent when shoe shopping and ask for assistance in finding the best fitting shoes for you. These are just some of many potential proactive foot care tips for seniors. For more, contact a podiatrist.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact Dr. James D. McAlexander from Gig Harbor Foot and Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in Gig Harbor, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

Of the 26 bones in the foot, the five long bones that connect the heel to the toes are the most frequently broken. These long bones, called metatarsals, can be injured in two ways: acute fractures and stress fractures. Acute metatarsal fractures can be caused by direct trauma to the foot, such as dropping something heavy on it or kicking a heavy object. Acute fractures are breaks in the bone. Stress fractures, on the other hand, are hairline cracks in the metatarsal, usually caused by repetitive use or overuse. They are common among runners, basketball players, dancers, and people who carry heavy packs while walking long distances. People with osteoporosis are also at risk for developing stress fractures. Symptoms felt with an acute metatarsal fracture are typically more severe than those from stress fractures. You may actually hear the crack as the bone breaks, and pain is immediate and specific. Movement of the foot will be difficult at best. With stress fractures, the symptoms develop gradually, starting out with general pain over a widespread area, which then becomes more and more noticeable. With either an acute metatarsal fracture or a stress fracture, it is imperative to see a podiatrist as soon as possible for an accurate diagnosis and treatment plan.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Dr. James D. McAlexander from Gig Harbor Foot and Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Gig Harbor, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
The human foot has 26 different bones, and the foot is divided into three parts: the hindfoot, the midfoot, and the forefoot. Each section of the foot is composed of a different amount of bones. For instance, the forefoot is made up of 19 bones. The midfoot is composed of five smaller bones called the navicular, cuboid, and three cuneiform bones. Lastly, the hindfoot is made up of only the talus and the calcaneus. The feet tend to be vulnerable to slipping and twisting; consequently, fractured bones within the foot are common. When a bone gets crushed, bent, twisted, or stretched it may become broken.
Many foot fractures occur through an accident or trauma. More specifically, common causes for broken feet are car accidents, falls, missteps, or overuse. If you have a broken ankle or foot, you may have one or more of the following symptoms: throbbing pain, swelling, bruising, tenderness, deformities, and difficulty walking.
There are some factors that may put you at a higher risk of developing a broken foot. People who participate in high-impact sports are more likely to develop foot fractures because of the stresses, direct blows, and twisting injuries involved in gameplay. Additionally, those who suddenly increase their activity level are more likely to suffer a stress fracture.
Unfortunately, there are different complications that may arise because of a foot fracture. For instance, arthritis may be caused by fractures that extend into the joints. Bone infections are also possible in open fractures due to the bone being exposed to bacteria. However, there are ways you can help prevent yourself from breaking your foot. One way to avoid fractures is to wear proper footwear. If you plan on going on a run, you should wear running shoes. You should also replace your shoes if you notice that they are becoming worn out. For runners, it is best to replace shoes every 300 to 400 miles.
Treatment for foot fractures usually consists of rest, ice, elevation, and compression (RICE). If you plan on wrapping your foot, try not to wrap it too tightly because doing so may cut off blood supply in the foot. You should also avoid walking on the fractured foot.
If you suspect you have a broken foot, you should see your podiatrist right away. It is important that you have someone bring you to your doctor, since driving with a broken foot can be dangerous. You should especially seek urgent care if you are experiencing numbness, pain, or deformities in your foot.
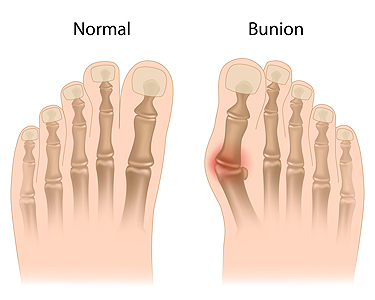
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
 Running is one of the most popular and widespread forms of exercise. Yet, bunions can often make this activity challenging or even painful. There are a variety of ways that individuals can manage the effects of bunions and continue to run. Bunions are bumps that occur usually on the base of the big toe when the metatarsophalangeal joint is stressed and strained. In some cases, bunions may form at the base of the pinky toe as well. If a runner has developed a bunion that is not causing serious pain, the runner may be able to continue running with wider footwear. Opting for wider running shoes can decrease the extent to which the bunion rubs up against the shoe and further aggravates or inflames the bump. Another way that runners may cope with bunions is by applying ice to the affected area for a short duration of time following the run. Toe spacers and bunion pads may also prove to be useful for runners looking to manage the annoyance of bunions. Bunions are certainly not ideal for runners, but a podiatrist may be able to help you address the affliction and get back on the running trail comfortably again.
Running is one of the most popular and widespread forms of exercise. Yet, bunions can often make this activity challenging or even painful. There are a variety of ways that individuals can manage the effects of bunions and continue to run. Bunions are bumps that occur usually on the base of the big toe when the metatarsophalangeal joint is stressed and strained. In some cases, bunions may form at the base of the pinky toe as well. If a runner has developed a bunion that is not causing serious pain, the runner may be able to continue running with wider footwear. Opting for wider running shoes can decrease the extent to which the bunion rubs up against the shoe and further aggravates or inflames the bump. Another way that runners may cope with bunions is by applying ice to the affected area for a short duration of time following the run. Toe spacers and bunion pads may also prove to be useful for runners looking to manage the annoyance of bunions. Bunions are certainly not ideal for runners, but a podiatrist may be able to help you address the affliction and get back on the running trail comfortably again.
If you are suffering from bunions, contact Dr. James D. McAlexander of Gig Harbor Foot and Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
If you have any questions, please feel free to contact our office located in Gig Harbor, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.